|
Did you join us at the FREE Beat Infertility Summit? If not- the good news is you can still register to attend the Summit here and have access to replays of over 60 informative talks from fertility experts across the globe. At the Summit we shared how essential your gut health is for fertility. Nurturing a health gut is one of the key steps we use with our clients for pregnancy success. Start with the Best Baby Making IngredientsThe single best predictor of a healthy embryo, that leads to pregnancy, is starting with a healthy egg and sperm. We can’t turn back time to be younger, but there are things we can do that are scientifically proven to benefit egg and sperm quality, AND create a receptive endometrium for implantation. We want our sperm to have great motility, morphology, for there to be enough of it (quantity) and for it to have low levels of DNA fragmentation or damage. We need our oocyte (egg) to look good and have functioning mitochondria inside so it has the ability to mature. We want a receptive uterus with good blood flow, ideal lining thickness and an immune response that is just right for implantation, not too much and not too little. Improving these ingredients in the baby making process does not start with your reproductive organs. It starts in your gut! Let’s explore the Gut-Fertility Connection, so you know how to leverage it for pregnancy success. Meet Your MicrobiotaWe have over 2kg of microorganisms or microbiota living in our gut (these are mainly bacteria). These microbiota produce essential vitamins, regulate our immune system, influence our metabolism, alter hormone levels, our muscle strength and even our mood. When our gut microbiota breakdown microbiota accessible carbohydrates, they produce these amazing short chain fatty acids. These short chain fatty acids are potent anti-inflammatory molecules. They enhance the barrier function of the gut cells and protect against pathogenic or bad bacteria. They can also regulate metabolism by influencing hormones involved in food intake and insulin secretion. Our gut microbiota are required to activate beneficial polyphenol compounds found in plant based foods and to ensure our immune system stays in check. Feeding Your MicrobiotaFeeding your gut microbiota is important and they love specific types of fibre – this makes them thrive! If they miss out on specific fibres, even intermittently, they can begin to breakdown the mucus layer of the gut as a food source. When the mucus layer of the gut is damaged, inflammation is increased and this ultimately damages eggs and sperm. Diet is the most potent modulator of your gut microbes. Nurturing them promotes greater diversity and the release of beneficial compounds that influence almost every process in your body. What you eat matters! Missing MicrobiotaIn many conditions affecting fertility, the gut requires some additional love. The diversity of the gut microbes is negatively impacted in PCOS, endometriosis, male factor infertility and unexplained infertility. There are higher levels of bad bacteria in the gut and low levels of beneficial bacteria that we need for optimal fertility. How do we improve the diversity of out gut microbes to optimise our chance of pregnancy? By feeding our microbes the food they need to thrive! What’s On My Plate? If you are wondering how to nurture your gut for optimal fertility, we would love you to join us in our first ever Fertile Gut Masterclass! Cut out the dietary noise and fast track your fertility by optimising your gut health. Over three weeks you will learn how to eat to nourish your gut for conception and beyond. This course delivers over $1200 value for the cost of less than one Consultation! What's that?! Yes- it's true BUT only for this first round offering!
Not only will this course improve your chance of conception with fertility treatment, but you may also improve your chance of natural pregnancy! The health of Mum and Dad to be at the time of conception influences the health of your future child so what better way to give your child the best start in life. If you want to give yourself the best chance of pregnancy success then this course is for you! Find out more about our Fertile Gut Masterclass Modules so you can create a fertile gut. There is a lot going on around the globe right now. We are in the midst of dealing with the emotional rollercoaster that is infertility as treatment cycles are postponed and the time frames for commencing treatment with COVID-19 restrictions remain uncertain. As we near the end of endometriosis awareness month, I wanted to provide some hope. Endometriosis is a condition where tissue of the endometrium is found outside the uterus. Twenty to 50% of women dealing with infertility have endometriosis [1]. For 20% of people seeking fertility treatment, endometriosis is the sole reason they require additional support to achieve pregnancy. Know that if you have endometriosis (my hand is up!), you are certainly not alone. While you wait, there are steps you can take to optimise your treatment outcome and chance of natural conception. While not all women with endometriosis have trouble getting pregnant, let’s look at how endometriosis affects fertility, and five steps you can take to give yourself the best chance of pregnancy success! Infertility with EndometriosisOxidative stress and inflammation are elevated in women with endometriosis [2, 3], and these overactive immune processes impact fertility. The increased oxidative stress and inflammation change the structure of eggs in women with endometriosis, making them less likely to mature once collected [4]. The endometrium is also different, which reduces embryo implantation and pregnancy progression. The good news? There are ways to dampen oxidative stress and inflammation! Changes in anatomy may also impact how likely egg and sperm are to get together. Over 30% of women with endometriosis may present with adhesions, which is a type of scar tissue [5]. Adhesions may cause structural changes that restrict the passage of eggs and sperm, making conception difficult. These adhesions are associated with increased pain, impacting quality of life [6] but there are positive ways to manage, and even reduce this pain. While fertility treatments for endometriosis may involve interventions like laparoscopic surgery, here are some steps you can take now to improve your chance of pregnancy success. Tips to Improve your Fertility with Endometriosis1. ExerciseOne of the best anti-inflammatories going around, exercise can play an important role in the management of endometriosis. Exercise ramps up anti-inflammatory and anti-oxidant defences to reduce inflammation. This improves the health of our energy producing mitochondria, hormone regulation and other pathways that promote better quality eggs. Exercise is also a powerful n effective tool for managing pain. Pain and depression are higher in women with endometriosis [7], but incorporating regular physical activity into your day can be a great way to improve quality of life and fertility! 2. Strength TrainMost people think of exercise as aerobic activities, such as walking or swimming, but don’t forget to strength train. Strength training promotes the production of anti-inflammatory proteins and can limit the loss of muscle and strength that comes with chronic exposure to high levels of inflammation. Getting strong is also a great way to boost energy levels to combat fatigue, and you can strength train from the comfort of your lounge room. 3. Nourish Your BodyA diet rich in different coloured fruits and vegetables, wholegrains and oily fish has been linked to a lower risk of developing endometriosis [6]. On the flip side, diets high in trans fats, which often come from processed foods, and low in anti-inflammatory Omega-3 fats may increase the risk of endometriosis [6]. If you have endometriosis, the good news is that diet is an incredible way to reduce inflammation and manage the condition. One strategy that may suit your medical history is to adopt a Mediterranean style of eating. This typically means:
Eating a Mediterranean Diet is effective for fertility as it changes what happens in your gut to optimise egg quality. See our next tip to find out more! 4. Improve Your Gut HealthWe have over 2kg of bacteria living in our gut. They influence how we get our nutrients from food, our mood, muscle strength and our fertility. In endometriosis, the growth of endometrial lesions outside of the uterus is driven by oestrogen, and our resident gut microbiota (the collection of bacteria and other microorgamisms in our gut) play a role in regulating these levels. Endometriosis is associated with an imbalance in gut microbiota. Women with endometriosis have lower concentrations of beneficial Lactobacilli bacteria, and higher levels of potentially pathogenic bacteria [8] that increase inflammation. You can promote a healthy balance of bacteria in your gut by eating a diet rich prebiotic fibre. Prebiotics act as a food source for beneficial gut bacteria. When you don’t get enough prebiotic fibre in your diet, your bacteria start to digest your gut lining for food, which promotes more inflammation. Eat a wide variety of fruits, vegetables and wholegrains each day to optimise your gut health for fertility. It can be hard knowing where to start and that’s where a specialist Dietitian can help! 5. Get to BedSleep is probably the single most important thing we can do to ensure physiological and mental health. Without sleep, our immune system is not as effective at fighting off viruses, our sex drive reduces, and our pain threshold increases. Research shows that sleep quality is reduced in endometriosis [9]. Missing out on sleep can reduce our pain threshold, and promote inflammation which we know is not great for fertility. Just as we adopt healthy habits around moving each day and making positive choices around what we eat, consciously adopt strategies that can improve your sleep. Stick to a usual bedtime and wake up schedule, avoid exposure to screens for an hour before bed and try a mindfulness app just as you get into bed to bring on sleep quicker. Once you are exercising regularly this has the benefit of enhancing sleep quality too! Get Empowered!Empower yourself to take charge of your fertility! If you would like extra support in getting started we are here to help. Make sure you are following us on Instagram at @DrKitic and @fertilegut for tips and strategies for improving your preconception health!
Factors affecting fertility include poor quality eggs and sperm, weight, sleep, metabolic elements, hormone balance and environmental exposures. Did you know that these are all influenced by what is happening in your gut? Our gut is the most important immune organ in our body. It is home to over 2kg of microbes that regulate lots of processes in the body. They talk to our brain, our muscles and can influence egg and sperm quality. The genetic material of our gut microbiome is more than 100 times ours so our complexity is not because we are human, but more likely because of the component of us that isn’t human. Having lots of different, beneficial populations living in our gut is associated with positive benefits for health and fertility. In contrast, when the populations in the gut are not as diverse or are out of balance, there are negative consequences for health and fertility. Read on to find out how our gut microbiota can be nurtured to enhance your fertility. Why Does our Gut Matter? Imbalances in our gut microbiota that lead to dysbiosis are associated with:
What is the Role of our Gut Microbiota? Our microbiota play a key role in extracting nutrients and energy from food, they influence how well our immune system works, they can protect us against bad bacteria and viruses and they can influence the strength of our gut barrier. A healthy, diverse gut microbiota is essential for a functional gut and fertility. Diversity Dampens Inflammation A diverse microbiota will ensure our immune system is working properly. Poor gut health is associated with an increase in microbiota that promote inflammation in the gut, which can then enter our bloodstream, impacting egg and sperm quality. Inflammation, and the resolution of inflammation, is usually a tightly regulated process if you gut is in good health. Controlled inflammation is essential for the repair of tissues, immune protection and even the process of implantation. While acute inflammation is a normal, healthy response to short-term stress or injury, chronic low-grade inflammation promotes infertility. Low diversity in your gut microbiota drives inflammation, which is not good news for fertility. Inflammation damages your gut lining and can lead to elevated levels of inflammation in your circulation. This then can cause damage to your developing eggs and sperm. Reducing inflammation is a proven strategy for enhancing your fertility. If your lifestyle nurtures a diverse microbiota you will keep inflammation in check and optimise your egg and sperm health. Extract More Antioxidants and Energy We started to understand more about our gut microbiota in 2006 when Jeffery Gordon (the father of the microbiome) demonstrated that the gut microbiota could control weight. He transferred the gut microbiota from obese mice to lean mice. The lean mice then put on body weight and increased fat mass despite consuming less food! In humans, differences in microbiota composition and diversity are observed between obese and lean individuals, showing that the gut microbiota plays a role. If you have been on antibiotics, this strips out your gut bacteria. With the changes in your gut populations you may have noticed that your health is not as optimal as it usually is or that you have put on weight despite a similar diet. Improving the diversity of your gut microbiota can help get you back on track. With a diverse gut microbiota we are able to activate polyphenols and other antioxidant compounds in the food we eat. Having a diverse, fertile gut means you may extract more essential nutrients from your food for optimising egg and sperm development. Boost Mental Health There are lines of communication between our gut and our brain. Over 16 years ago a study in mice showed that when mice were exposed to stress, the magnitude of their physiological response was dependent upon their gut microbiota. Certain strains of bacteria have been shown to reduced anxiety- and depression-like behaviour and the gut microbiome can shape how our brain functions, even altering neurotransmitter production. Anxiety and depression are common in women and men dealing with infertility. An imbalance, or dysbiosis, of the populations living in the gut can impact our brain and our behaviour. Nurturing our gut microbiome for enhanced diversity can provide many benefits for your mental wellbeing. Have you head the term “Food and Mood” or “Move for Your Mood”? What we eat and how we move our bodies are key regulators of promoting a diverse microbiota for better mental health. Looking to build resilience? Want to reduce the anxiety and stress around trying to conceive? Optimal nutrition to fuel your gut diversity and the ideal exercise prescription are essential tools for pregnancy success. Reduce Toxin Exposure Our fertility can be affected by certain chemicals. For example, exposure to Bisphenol A or BPA reduces egg and sperm quality and may account for 20% of unexplained infertility. BPA can be rapidly broken down in the gastrointestinal tract by certain microbes. If you are lacking these microbes, or their populations are small, your absorption of BPA will be greater, leading to more endocrine disruption. Having a diverse gut microbiota appears to be protective against certain chemicals that damage fertility. Greater gut diversity means less absorption of these harmful chemicals. Ways to Nurture your Microbiota In working with our clients for pregnancy success we have a focus on proven strategies that will improve gut diversity as it is central to fertility. Shaping a fertile gut microbiota depends on the availability of microbiota-accessible carbohydrates that are found in dietary fibre. Prebiotics are an important type of fibre. They are nondigestible, fermentable foods and you may already eat them every day. Prebiotic fibre has distinct physical and chemical properties which interact with the microbiota of your gut to benefit fertility. Our microbiota thrives on prebiotic fibre and one of the reasons why, is that it enables them to make the short-chain fatty acid butyrate. Butyrate is incredibly potent at dampening inflammation, strengthening the gut barrier, regulating metabolism, optimising brain health and regulating immune function. The mechanisms of action of butyrate are incredibly beneficial for fertility as they dampen processes we know compromise egg and sperm quality and the progression of a healthy pregnancy. Getting a variety of fibre in your day is a promising strategy for weight management, reducing the risk of metabolic disease and improving your reproductive health! Keep up the intake of fresh, wholefoods that are packed with prebiotic fibre. If you can't seem to get enough variety in your day, you are trying to conceive, or you just can't get organised for a veggie laden meal, then top up your diet with the proven mix of prebiotic fibres and Omega-3 in Fertile Gut. Want to Improve Your Gut Health for Pregnancy Success?Get in touch with us to find out more about how we can enhance your preconception health. Find out if we are the right support for you by booking in a FREE 10 min phone call with us.
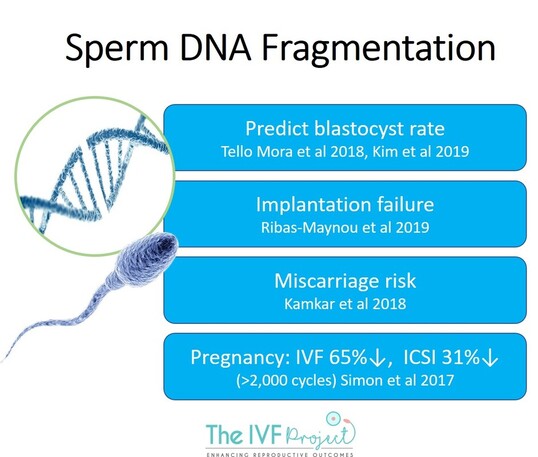
Investing in developing the best quality eggs and sperm will give you the best chance of success and we are here to help! [email protected] Male infertility is the main reason around 40% of couples seek fertility treatment. In assessing male fertility, semen analysis is the most important test. While this visit to the 'specimen collection room' is unavoidable, this initial assessment does not necessarily capture your potential for pregnancy. Routine semen analysis will count the number of sperm and check their shape (morphology) and movement (motility), there is one thing it does not measure: DNA fragmentation. Today I want to share with you what DNA fragmentation is, why it matters and what you can do about it! What is Sperm DNA Fragmentation? DNA is essentially the genetic instruction book for how we grow and function that is contained in every living cell. Breaks, or fragmentation, of the DNA will affect how the cell functions. A small amount of DNA damage is always present but when this damage is high, fertility is reduced. If your viability is low (<50%), then it is likely that you have high DNA fragmentation rates [1]. Even with a normal semen analysis, 15% of men can have high levels of DNA damage to the sperm. DNA fragmentation is a major factor in unexplained infertility. Does Sperm DNA Fragmentation Reduce Our Chance of Pregnancy?High levels of sperm DNA fragmentation:
While semen analysis may be normal and you may have good fertilisation of your collected eggs, if you have multiple transfers that don’t implant or recurrent early pregnancy loss, DNA fragmentation may be a factor. When a sperm with DNA damage fertilises an egg, the egg has to invest energy trying to repair the damaged DNA. If there is lots of DNA damage, the embryo won’t have enough energy to develop normally. This leads to an inability to implant or to develop further once an embryo has implanted. In an ideal situation you want your embryo spending time growing and developing, not repairing itself from the outset! What Causes Sperm DNA Fragmentation?Inflammation and oxidative stress are drivers of DNA fragmentation. Inflammation and oxidative stress are elevated with poor diet, insufficient or very high levels of physical activity, stress, sleep deprivation, alcohol and chemical exposure (just to name a few). How Can I Lower Sperm DNA Fragmentation? One of the most potent ways to reduce sperm DNA fragmentation is by exercising regularly at optimal intensities with enough recovery. Infertile men completing a progressive structured running program over 24 weeks had significantly reduced levels of sperm DNA fragmentation. Inflammation and oxidative stress were also significantly lower but best of all these men had a significant increase in pregnancy rate when compared to a non-exercising control group [2]. Structured resistance training also significantly lowers DNA fragmentation [3]. Where Do I Begin?If you are exercising regularly you may want to check in with an Accredited Exercise Physiologist that your current routine is supporting optimal sperm health. The intensity, frequency and duration of your exercise sessions in combination with your strength training can be optimised for creating healthy sperm. If you have yet to get moving, make sure you get expert advice from and an Accredited Exercise Physiologist so you can ensure you get the best prescription that is tailored for your individual needs and for making your sperm the best it can be! Sperm takes ~72 days to be produced so changes you make now will produce healthier, happier sperm in as little as 12 weeks. It's time to get moving! References
1. Samplaski, M.K., et al., The relationship between sperm viability and DNA fragmentation rates. Reprod Biol Endocrinol, 2015. 13: p. 42. 2. Maleki, B.H. and B. Tartibian, High-Intensity Exercise Training for Improving Reproductive Function in Infertile Patients: A Randomized Controlled Trial. J Obstet Gynaecol Can, 2017. 39(7): p. 545-558. 3. Hajizadeh Maleki, B. and B. Tartibian, Resistance exercise modulates male factor infertility through anti-inflammatory and antioxidative mechanisms in infertile men: A RCT. Life Sci, 2018. 203: p. 150-160. I hear of so many people removing gluten from their diet in a bid to improve their fertility and get pregnant. There is a lot of misinformation out there so here is a wrap of gluten and fertility to get informed about the decisions you make! What is Gluten? Gluten is essentially the ‘glue’ that holds cereal grains together. It is a protein found in wheat, rye, barley, oats and anything derived from these gluten containing grains such as malt. Gluten is a common additive to many foods (sometimes as a thickener or colour) so you may find it in ice cream, lollies, processed meats, yoghurt and salad dressings. For those diagnosed with Coeliac Disease, eating gluten disrupts the gastrointestinal tract and damages intestinal cells, stressing the immune system and reducing the absorption of nutrients. Untreated Coeliac Disease is a cause of ‘unexplained’ infertility but the number of women with undiagnosed Coeliac Disease is low. In a recent Canadian study, only 1.2% of women with unexplained infertility were diagnosed with Coeliac Disease following routine screening (1). If you are a Coeliac then removing gluten from your diet will improve your fertility. If you are not a Coeliac, there is no scientific evidence to support that eating gluten free will improve your chance of pregnancy. It can be exhausting reading food labels to determine if a product is gluten free but for anyone diagnosed with Coeliac Disease, a strict gluten free diet is the only management strategy we currently have. There is hope that hookworms may help but expect any alternative treatment to be at least a decade away. As a Coeliac myself I am hopeful that one day I can eat some gluten containing goodies! Is it Gluten or FODMAPS? Some people who are not diagnosed with Coeliac Disease experience symptoms such as abdominal pain, diarrhoea, bloating and excessive wind and fatigue that they attribute to eating gluten or wheat. This has been termed ‘Non-Coeliac Gluten Sensitivity’ and emerging research in this field suggests that it is not gluten that contributes to these symptoms but rather the FODMAP content of the diet (2). FODMAPs are short chain carbohydrates that may be poorly absorbed in the gastrointestinal tract. FODMAPs include fructose (when in excess of glucose), fructans, galacto-oligosaccharides, lactose and polyols (eg. sorbitol and mannitol) – hence the acronym! Some of our work in healthy athletes has shown that reducing dietary FODMAPs can reduce gastrointestinal symptoms (3) so it may not be gluten that is the culprit if you are experiencing gastrointestinal distress. If you think you need to remove gluten from your diet make sure you find the cause of your symptoms with a proper medical diagnosis prior to gluten removal. Is Eating Gluten Free Healthier? Somehow ‘gluten free’ has become synonymous with ‘healthy’, but is eating gluten free actually healthier? If processed foods are removed from your diet and you eat more whole foods when eating gluten free, then generally this will be associated with a reduction in dietary intake of sugars and saturated fats (including trans fats) which would be beneficial to health and fertility. But, there may be some other dietary changes associated with removing gluten that are not so great for health, especially if you reduce your intake of grains. Removing gluten from your diet by cutting out bread, pasta and cereal may significantly reduce your dietary intake of fibre (which has neagtive consequences for creating a Fertile Friendly Microbiota) and carbohydrate. Carbohydrates are a really important component of a balanced, healthy diet and importantly wholegrain intake has been associated with improved outcomes for fertility treatment (4). Gluten containing grains are often substituted for carbohydrate rich but protein poor ingredients such as maize starch, white rice flour, potato starch or tapioca starch in gluten free alternatives. This means that your protein intake could be reduced, which may impair fertility. A study that investigated the nutritional value of over 3000 gluten free and non-gluten products in 10 categories of food showed that relative to non-gluten free foods, gluten free products had consistently lower average protein content (5). When you consider that gluten free products often substitute ingredients with low fibre and protein alternatives, and that gluten free products may contain more sugar and fat to improve taste, eating gluten free is not necessarily a healthier option. Does Gluten Influence Thyroid Function? There is a partial genetic overlap between Coeliac Disease and autoimmune diseases. If you have Coeliac Disease, you are four times more likely to have an autoimmune thyroid disease. If you have been diagnosed with hypothyroidism you should immediately undergo clinical investigations for Coeliac Disease. A first step in this process is screening for blood levels of antibodies to gluten. If you have removed gluten from your diet before any investigations you will need to start eating gluten again for a period greater than one month so you can receive an accurate diagnosis. While there is a link between Coeliac Disease and an increased prevalence of autoimmune thyroid disease, there is no evidence to support a link between eating gluten and an increased risk of thyroid issues. Indeed, even in people with Coeliac Disease that is undiagnosed, the duration of exposure to gluten is unrelated to the risk for autoimmune disease. To date, there is no scientific evidence to support removing gluten from the diet as a treatment strategy for thyroid disorders (unless of course you are a Coeliac). Hypothyroidism and Coeliac Disease are associated with reductions in egg quality and infertility (6,7) so getting a proper diagnosis is paramount. While removing gluten may not be the answer, diet can influence thyroid function and resulting metabolism. Dietary protein intake has been linked to thyroid function in a number of animal studies, with low protein diets reducing thyroid function, increasing abdominal obesity and impairing glucose regulation (8). Ensuring adequate protein in the diet has potential to improve thyroid function and adequate protein intake is essential for muscle building too. Some foods such as broccoli, cabbage, cauliflower, brussel sprouts, turnips, walnuts, almonds and soy may limit iodine availability, although this is only if consumed in large amounts. Cooked cruciferous vegetables in moderate amounts pose minimal risk for thyroid health (9) and given the other micronutrients they contain, their intake along with adequate iodine will form part of a balanced diet. What's Your Gut Feeling? The immune stimulating potential of gluten may be related to your gut microbiota. The HLA-DQ9 gene is the most commonly linked to Coeliac Disease yet some people carrying the gene do not have Coeliac Disease. Could the resident bacteria in your gut influence your propensity to develop Coeliac Disease or Non-Coeliac Gluten Sensitivity?
A study using mice looked at the impact of the gut microbiome on the response to gluten (10). Three groups of mice with three different microbiomes (different populations of bacteria and yeast in the gut) were exposed to gluten for two weeks. Mice with no microbiome (germ free) and mice with a microbiome that contained a number of disease causing species developed an adverse response to gluten, while mice with a healthy microbiome (free of disease causing pathogens) did not have an adverse response. There may be value in ensuring your microbiome is in top shape! Historically, a gluten free diet has been associated with sub-optimal intake of protein, fiber, B vitamins, and iron alongside increased fat and sugar intake (11). In combination with possible micronutrient deficiency, removing gluten may have other adverse consequences. In healthy adults adhering to a gluten free diet for one month, numbers of healthy gut bacteria decreased while numbers of unhealthy bacteria increased. Rather than removing gluten from your diet, if not medically necessary, a focus on pre-biotic foods and eating a variety of fresh whole foods is sure to confer more benefit. Are you getting enough prebiotic foods in your day? References 1. Gunn, B., Murphy, K.E., andGreenblatt, E.M. (2017). Unexplained Infertility and Undiagnosed Celiac Disease: Study of a Multiethnic Canadian Population. J Obstet Gynaecol Can. 2. Biesiekierski, J.R., Peters, S.L., Newnham, E.D., Rosella, O., Muir, J.G., andGibson, P.R. (2013). No effects of gluten in patients with self-reported non-celiac gluten sensitivity after dietary reduction of fermentable, poorly absorbed, short-chain carbohydrates. Gastroenterology 145(2): 320-8 e1-3. 3. Lis, D.M., Stellingwerff, T., Kitic, C.M., Fell, J.W., and Ahuja, K.D.K. (2018). Low FODMAP: A Preliminary Strategy to Reduce Gastrointestinal Distress in Athletes. Med Sci Sports Exerc 50(1): 116-123. 4. Gaskins, A.J., Chiu, Y.H., Williams, P.L., Keller, M.G., Toth, T.L., Hauser, R., Chavarro, J.E., andTeam, E.S. (2016). Maternal whole grain intake and outcomes of in vitro fertilization. Fertil Steril 105(6): 1503-1510 e4. 5. Wu, J.H., Neal, B., Trevena, H., Crino, M., Stuart-Smith, W., Faulkner-Hogg, K., Yu Louie, J.C., andDunford, E. (2015). Are gluten-free foods healthier than non-gluten-free foods? An evaluation of supermarket products in Australia. Br J Nutr 114(3): 448-54. 6. Meng, L., Rijntjes, E., Swarts, H., Bunschoten, A., van der Stelt, I., Keijer, J., andTeerds, K. (2016). Dietary-Induced Chronic Hypothyroidism Negatively Affects Rat Follicular Development and Ovulation Rate and Is Associated with Oxidative Stress. Biol Reprod 94(4): 90. 7. Tersigni, C., Castellani, R., de Waure, C., Fattorossi, A., De Spirito, M., Gasbarrini, A., Scambia, G., andDi Simone, N. (2014). Celiac disease and reproductive disorders: meta-analysis of epidemiologic associations and potential pathogenic mechanisms. Hum Reprod Update 20(4): 582-93. 8. Palkowska-Gozdzik, E., Lachowicz, K., andRosolowska-Huszcz, D. (2017). Effects of Dietary Protein on Thyroid Axis Activity. Nutrients 10(1). 9. Felker, P., Bunch, R., andLeung, A.M. (2016). Concentrations of thiocyanate and goitrin in human plasma, their precursor concentrations in brassica vegetables, and associated potential risk for hypothyroidism. Nutr Rev 74(4): 248-58. 10. Caminero, A., Galipeau, H.J., McCarville, J.L., Johnston, C.W., Bernier, S.P., Russell, A.K., Jury, J., Herran, A.R., Casqueiro, J., Tye-Din, J.A., Surette, M.G., Magarvey, N.A., Schuppan, D., andVerdu, E.F. (2016). Duodenal Bacteria From Patients With Celiac Disease and Healthy Subjects Distinctly Affect Gluten Breakdown and Immunogenicity. Gastroenterology 151(4): 670-83. 11. Theethira, T.G., Dennis, M., andLeffler, D.A. (2014). Nutritional consequences of celiac disease and the gluten-free diet. Expert Rev Gastroenterol Hepatol 8(2): 123-9. We all too often hear about the decline in fertility with female age but little attention is given the other 50% of the equation. A father’s health prior to conception can influence pregnancy progress and their future child’s health. It sounds a bit far fetched that your current health can have an impact on future generations but that is the science of epigenetics! And like most things, this can be for good if you are looking after yourself with a healthy lifestyle, or for bad if your health is not getting the attention it needs. What the Heck is Epigenetics? Epigenetics is essentially the modulator and interpreter of your DNA. DNA is our inherited genetic material, but epigenetics can change the way that our genes are turned up or turned down. Lifestyle is a key regulator of these chemical messages that can turn a gene on or off so you can appreciate how important exercise, sleep, diet and stress are influencing our health. If you would like to read more about epigenetics check out this article at the Australian Academy of Science. Why Does Age Matter? As men age there is a decrease in fertility and an increase in pregnancy complications such as gestational diabetes, low birth weight and preterm birth. The children of fathers over 45 years have increased risks of chromosomal and non-chromosomal birth defects and has been linked to an increased incidence of childhood autism and cancers. One reason for the decline in fertility is that with age comes a decrease in the key male sex hormone testosterone. As testosterone levels decline sperm quality is reduced and in a double whammy, it is likely that libido is reduced too. Can You Turn Back the Clock? While you can’t change your chronological age, there are some great strategies to reduce the impacts of ageing on fertility.
Endurance exercise like jogging, cycling and swimming is key for driving anti-ageing changes at the cellular level. Regular aerobic exercise at the optimal intensity will dampen oxidative stress and inflammation, ultimately influencing the expression of your genetic material within the cell so you can pass on positive health traits to your future offspring. Resistance training twice a week is also a great way to increase testosterone concentrations that may decline with age. Aerobic exercise helps raise testosterone by reducing body fat levels (which reduce fertility) but a strength training session will raise testosterone concentrations immediately, improving sperm health. Aim to strength train all major muscle groups at least twice a week. How is YOUR sperm health? Never underestimate the power of positive thinking, and while you are imagining your little embryo implanting to become a big fat positive (BFP) there are some positive steps you can take to get that egg to stick! Time to put your feet up? I have read some advice suggesting that women have complete bed rest for two days after their transfer. PLEASE NO!!! While it is not the time to run a marathon, everything we know about the negative effects of bed rest for physiology and your mental state suggests that this would be detrimental. The concept of bed rest stems from old school thinking that the contents of your uterus will fall out as soon as you stand up and walk. Hmmm... no. Studies that have used ultrasound to track air bubbles delivered into the uterus have shown that 15 minutes of walking straight after transfer had no effect on the uterus contents so it is safe to say that your embryo will not fall out. Ban the bed rest Excitingly a systematic review (scientific analysis of all literature on the topic) exploring the effects of bed rest after embryo transfer and the outcome of IVF/ICSI has recently been published – and guess what? Bed rest is NOT GOOD. The review included studies involving autologous transfers (women’s own eggs) and varied fertility issues such as oligomenorrhea (infrequent menstrual periods), endometriosis and male factor infertility. In one study included in the review the patients were even catheterized so they didn’t have to get up and go to the toilet! Who has two days to hang around in bed?? Anyway, prolonged bed rest (24 hours) was found to be associated with lower rates of clinical pregnancy. Women who rested in bed were 40% less likely to have a Big Fat Positive (pregnancy test) (1). So if bed rest, or a marathon, is not on the menu then what should you be doing? The IVF Project can guide you during this two week wait with your individualised exercise prescription! Reference
1.Craciunas L, Tsampras N. Bed rest following embryo transfer might negatively affect the outcome of IVF/ICSI: a systematic review and meta-analysis. Human fertility (Cambridge, England). 2016; 19: 16-22. Polycystic ovary syndrome (PCOS) is a common endocrine disorder that affects 5-20% of women of reproductive age worldwide. PCOS is characterised by increased levels of androgen hormones such as testosterone and menstrual / ovulatory dysfunction. It is frequently accompanied by insulin resistance and obesity, resulting in a high risk for type 2 diabetes and cardiovascular disease. Losing body weight when you have PCOS is difficult – and it should not be your primary focus. Focus instead on moving regularly (sit less) and eating a wide variety of fresh, unprocessed food which will have a real impact on improving your fertility. Lifestyle Modification Works! Ovulation rates improve dramatically in women with PCOS after adopting an active lifestyle and eating a nutritionally balanced, energy restricted diet [3, 4]. Live birth rates also more than double! [3]. Delaying fertility treatment to give yourself time to be the healthiest you can be is associated with improved assisted reproductive treatment outcomes. Research shows that differences in the expression of progesterone receptors in the endometrium of women with PCOS could impact upon embryo implantation. The right exercise prescription can restore balance to the menstrual cycle, and in particular women with PCOS can realize benefits of improved blood glucose control and insulin resistance, even without weight loss. Exercise can also restore progesterone receptors in the endometrium, which can benefit embryo implantation. At a minimum, a three-month investment in making positive lifestyle changes that include exercising right could save you treatment cycles (which translates to saving your emotional sanity and money). It’s no wonder that Medical Research Guidelines state that exercise should be first line therapy for all women with PCOS. If you conceive, this is just the start of a very long journey where your health has a direct influence on not only the health of your pregnancy but your child’s health. Exercise during pregnancy reduces gestational diabetes, low back pain assists with gestational weight control and reduces the need for a caesarean section (C-section). Exercise during pregnancy also boosts newborn brain development so start planning not just for the timing of your trigger shots but for a healthy pregnancy and beyond. Feeling Hungry? Our brain plays a key role in regulating food intake along with our gut and fat tissue. These communication channels involve a number of hormones to relay messages and there is evidence that two of these hormones, insulin and neuropeptide Y, are differently regulated in PCOS [5]. Insulin is a hormone secreted from the pancreas that plays an important role in regulating our blood sugar levels, and energy (fat) storage. When we eat foods containing carbohydrate, the carbohydrate is broken down to glucose and absorbed into the bloodstream. The glucose provides fuel for our body and almost every cells needs glucose to function. Insulin is required for cells to take up glucose or to store glucose for later. Cells have special receptors to recognise insulin which will then ‘open the door’ for glucose to enter the cell. If the cells have fewer insulin receptors than normal or they are not working properly, they are described as insulin resistant. Without glucose getting into the cells, the pancreas works overtime to produce more insulin, leading to high levels in the blood. When the cells do not respond as they should to insulin and the pancreas produces more and more insulin, this is described as ‘insulin resistance’ that over time leads to diabetes. One way to lower insulin levels in the blood is to ensure your diet is designed to reduce insulin levels by incorporating the right amount and type of carbohydrate. Another way to lower insulin is to ensure you are engaging in regular physical activity. We can provide you with your personalised exercise program and comprehensive dietary feedback from your nutrition analysis to give you the best chance of conception! There is also evidence that in PCOS the usual concentrations and response to Neuropeptide Y is affected. Neuropeptide Y initiates appetite drive so typically levels are elevated during periods of food restriction. In PCOS, levels of this hormone have been reported as both lower than normal [6] and higher than normal [7] and may contribute to the reduced feeling of fullness and increased hunger following a meal in women with PCOS when they are compared to healthy women[8]. When hormone levels are low for prolonged periods the body sometimes become hypersensitive to the hormone so it takes far less hormone to stimulate a response than normal. Low levels of neuropeptide Y could increase the body’s sensitivity to the hormone, increasing appetite. Similarly, high levels of neuropeptide Y reported in PCOS women would also stimulate appetite. Insulin concentrations can regulate neuropeptide Y so strategies to reduce insulin levels will also modulate appetite. For this reason (and many others), exercise and nutrition are key in the treatment and managements of PCOS [9]. Where to Start? Lifestyle change can improve your chance of pregnancy by over 200%. To get the best, evidence based guidance book in your initial consultation with Dr Kitic for access to our fertility specialist practitioners who will take you on a step by step journey to enhance your reproductive health!
It’s the New Year! Despite this been the time that some people sit down and write a list I must admit that I’m not one for making New Year resolutions.
If I realise something I need to be doing to improve my wellbeing, personal or professional growth, I find planning a strategy to incorporate this into every day life is far more effective than an unrealistic New Year resolution. Working out how you can improve aspects of your health can seem overwhelming but there are often small things we can do each day that will take us in the right direction. Change does not always have to be drastic as over committing may see you set yourself up for failure and back at square one. Little things such as taking the stairs when you have the opportunity and getting to bed earlier are great starters. Building healthy habits into your daily routine will not only improve your long term health but also benefit fertility! You may want to start the year with a process of self-reflection to help guide you in what you plan for the New Year. What went well in 2018? What constructive and positive elements do you want to carry over into 2019? What didn’t work so well in 2018 and what are you looking to change in the New Year? What elements can you take control of to reach your goal? A great exercise to include in this self-reflection is an oldie but a goodie- the pros and cons list! This can be considered like a balance sheet for weighing up how important change is to you and also letting you know what habits you don’t want to let go of! Get out a pen and a clean sheet of paper that you divide into three columns. For an example of how to fill out the sheet, we can focus on a health behaviour where someone may not be regularly exercising (we could consider regular as a minimum of 3 aerobic sessions a week plus two strength sessions) write down in the first column “staying sedentary” and then you can put the pros (all the positives) of that behaviour in the second column and then write the cons (any negative consequences) associated with that behaviour in the third column. Beneath this they would write an alternative behaviour such as “exercising regularly”. They would then list all the pros and cons associated with this behaviour. Think about any behaviours you have thought about changing or that you know may be holding you back. Once you have your own table complete, take some time to contemplate the pros and cons of each behaviour and see if you have some clarity around where you will focus your energies for 2019. Plan little changes into your current daily routine to give yourself every chance of success and may 2019 be your year! Does this sound familiar? I found myself saying this last week so it’s a good time to anticipate that at some point you may be feeling this way, or have you already said 'I'm too tired to exercise'? The desire to give yourself the best chance of conception and set routines for a healthy pregnancy and baby may be all the motivation you may need to get moving but some days this can be a challenge. Some tips here may help you find that extra incentive! What Physical Activity Makes you Feel Good?This could be an interval session with some high intensity exercise, a Pilates session that really challenges your core or a quick walk outdoors among fresh air and greenery. It is so rare not to feel better after some exercise so when I feel tired and just want to sit down rather than get moving I go straight to my inner monologue that reminds me how good I feel afterwards. Exercising is like an instant mood lift – even if it’s a quick lounge room strength workout you will almost always feel better for doing something rather than nothing. Regular Exercise Actually Increases Energy and Reduces Fatigue.If you find yourself too tired this is when you really need to be exercising! The vitality boosting quality of exercise is why it is an effective component of treatment for conditions associated with fatigue such as cancer, where exercise improves fatigue, enhances sleep quality and even reduces depression. As you look forward, these benefits will also carry over to a healthy pregnancy. Women who resistance train experience less fatigue, better sleep quality and more energy during pregnancy. Fit in Your Workout First Thing. Resist hitting snooze and put on your workout gear as soon as your feet hit the floor out of bed. Do a quick lounge room workout, fit in your gym session or a walk before you start the rest of your day. YOU are incredibly important and looking after your physical and mental health will be a great asset on your fertility journey. Are you Getting Enough Sleep? While you are out hitting the pavement or doing some strength exercises contemplate WHY you may be feeling tired. We know that sleep is one of the most important tools for physical and psychological health. The amount of sleep we get impacts our production of hormones, how we regulate blood sugar and can also affect our weight.
It is not too much of a surprise then that missing out on quality sleep can also affect our fertility. Sleep disruption, or not getting enough sleep, can alter levels of reproductive hormones, affecting ovulation, endometrium receptivity and libido! Aim for 7-8 hours of undisturbed sleep a night. A great excuse to hit the pillow early! |
|
1300 084 694
[email protected] Suite T36, 477 Boundary St Spring Hill, Brisbane QLD 4000 Fax. 07 3540 8164 Copyright © 2022
|